Oggie, Oggie, Oggie Oi, Oi, Oi
Oggie is back with his next epic challenge, set to hit 800 official marathons within 800 weeks and donate £800 to help vital mental health services in Northern Ireland. All of this just days after he celebrates his 68th birthday on 1 May 2025, when he runs this year’s Moy Park Belfast City Marathon for Action Mental Health again.
From competing in the Belfast City Marathon last year where he achieved his 250th sub 4hr marathon for Action Mental Health out of his total at the time, which then stood at 740 official marathons, he has since added another 60 official marathons to this total. This will amount to 800 on the day of the Belfast City Marathon on Sunday 4 May 2025.
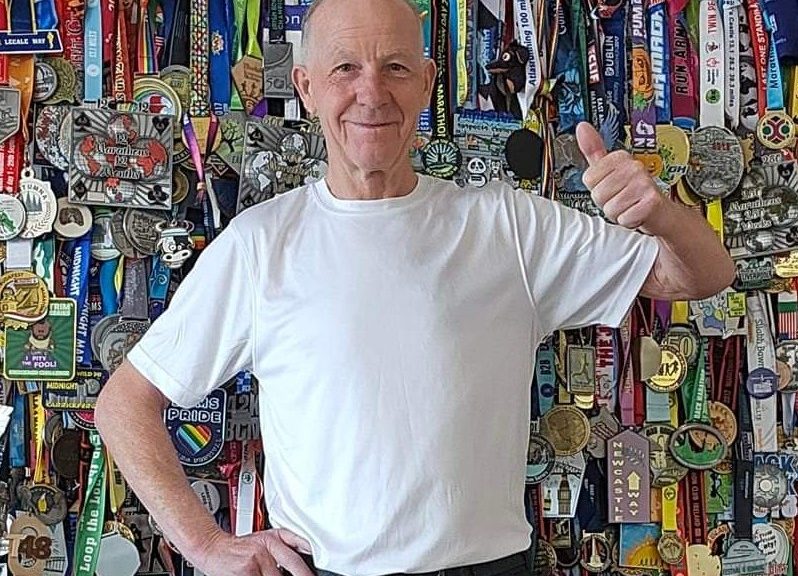
As well as being such a long-time supporter of Action Mental Health, Oggie has also ran a lot of marathons for other charities, including:
World Cancer Research, Action Cancer, Age Concern, Air Ambulance, Southern Area Hospice, McMillan Cancer Support, Foyle Hospice, PIPS, Marie Curie Cancer Care, The Donkey Sanctuary, Simon Community, Aware, Multiple Sclerosis Society, Northern Ireland Hospice, The Rainbow Project and Pretty in Pink.
This year, just one week before Belfast City Marathon, Oggie has also ran the London Marathon on 27 April. He revealed,
“I feel quite blessed and lucky that I am fit enough to always qualify for the bigger major marathons” explaining that he does not have a coach or a personal trainer, preferring to conduct the hard training work under his own steam in all weather conditions.
With a strict and demanding training regime, Oggie looks to future potential achievements with a measured approach saying,
“I take each day at a time and while I train on a daily basis and keep myself at optimum fitness, I’m realistic about my goals and how I may achieve them. I ran my first marathon on my 55th Birthday, which was at the Belfast City Marathon in 2012 and I had no prior sporting history before this time, not even in my school days. I know how important exercise in general is for mental health; it’s great for mind, body and soul. Aside of my accomplishments, if I can encourage others to make sport a part of their lives, even in a small way, I will have achieved my greatest goal of all.
Adding, “We all need encouragement, it’s just that important; runners share and help one another, and I’m often asked how I do it. To this day other runners and bystanders all give me the inspiration to keep going.”

Jonathan Smyth, Head of Communications & Fundraising, Action Mental Health said: “As a loyal supporter of Action Mental Health, Oggie reached out once again to let us know about his new personal challenge and we are absolutely thrilled to have his support and generosity once again. Oggie has pledged to donate £800 to support our vital mental health services, when he completes his challenge. We know that running, and indeed all physical activity is a great way of supporting your mental health, so we are particularly delighted to be the beneficiary of this amazing challenge and we wish Oggie well.”
In conclusion, Oggie said,
“I hope that my efforts will inspire other people to become active. I firmly believe exercising and keeping active can help not just our physical health but our mental health too. This is why I thought what better way to celebrate than to donate money from the Moy Park Belfast City Marathon to Action Mental Health, to help support the important work they do across Northern Ireland.”
If you feel inspired by Oggie’s story, run today for someone’s brighter tomorrow. Join #TeamActionMentalHealth and raise vital funds for mental health services in Northern Ireland. For more information, email [email protected].